The Connection Between Pain and Mental Health
Chronic pain significantly impacts your mental and emotional well-being. We understand that pain can bring along feelings of frustration, anxiety, and depression. These emotional factors can amplify the experience of pain, making it feel more intense and harder to manage. That’s why we integrate behavioral health support as part of our interventional pain management approach.
Our behavioral health program is led by Dr. William Schiff, a licensed psychologist with over 20 years of experience in the field of clinical and health psychology. Dr. Schiff is passionate about helping individuals dealing with chronic pain, disability, and illness. His approach considers the biological, psychological, and social factors that contribute to pain. He works closely with our pain management specialists to create a plan that not only addresses the physical aspects of pain but also focuses on improving your emotional and mental resilience.
Behavioral health support at Augusta Pain Center aims to help you break the cycle of pain and improve your overall quality of life.
How Behavioral Health Supports Pain Management

At Augusta Pain Center, we believe in a comprehensive approach to pain management, one that recognizes the important role mental and emotional health play in your recovery. Our experienced behavioral health team works closely with our pain management providers to integrate therapeutic strategies that can enhance your overall treatment plan.
These behavioral health techniques are designed to help you:
- Reduce stress by practicing relaxation and mindfulness exercises.
- Shift negative thinking patterns through cognitive-behavioral therapy (CBT), which can help you manage emotions and stay positive despite chronic pain.
- Increase your tolerance for pain using biofeedback, which teaches you how to control physiological responses to stress and discomfort.
- Improve your quality of life by teaching coping strategies to deal with daily pain in a healthy way.
By incorporating these practices into your treatment, we aim to provide you with the tools needed to improve both your mental and physical well-being. Together, these approaches can boost your overall resilience, making it easier to tackle pain from all angles.
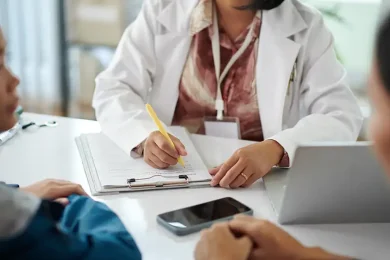
What to Expect from a Behavioral Health Evaluation
Behavioral health evaluations at Augusta Pain Center are an essential part of our approach to creating individualized treatment plans. This evaluation allows us to learn more about your emotional and psychological well-being, which helps us understand how pain is impacting you on a deeper level. It’s not about judgment or assigning blame—it’s about understanding the full picture of what you’re going through so we can help you move forward with a comprehensive plan that’s tailored to your unique needs.
During your evaluation, you may discuss topics such as:
- Your pain history and how it affects your daily life.
- Emotional factors, such as any stress, anxiety, or depression that might be present.
- Your coping mechanisms and any challenges you’ve faced in managing pain.
- Your support system, which can help inform your treatment plan.
Additionally, the law requires due diligence when prescribing narcotic pain medications, and a behavioral health evaluation helps your provider identify any concerns that could be a barrier to prescribing these types of medications.
After the evaluation, your pain management specialist will work with you and Dr. Schiff to outline a treatment plan that helps address both the physical and emotional aspects of your pain. This collaborative effort gives you the best chance for long-term relief and improved quality of life.
Ongoing Support for Chronic Pain

Living with chronic pain can often feel isolating, but you don’t have to face it alone. At Augusta Pain Center, we offer a Chronic Pain Support Group to provide a safe and supportive space where you can connect with others who understand exactly what you’re going through. This group is led by trained professionals and designed to offer both educational guidance and emotional support, giving you practical tools to manage pain and cope with its challenges.
In the group, you’ll have the opportunity to:
- Share your experiences and hear from others who are walking similar paths.
- Receive education on pain management techniques, stress reduction, and healthy coping strategies.
- Gain emotional support from others who truly understand the psychological and emotional impact of chronic pain.
- Learn from expert facilitators who can guide you in managing pain and living a more fulfilling life despite your challenges.
If you’re interested, please call us at (706) 738-7246 to RSVP. Joining the group can provide the sense of connection and validation that many people living with chronic pain need, helping you feel empowered to manage your journey.